Table of Contents
The Renin-angiotensin system is a physiological hormone system involved in regulating arterial blood pressure and sodium concentration in plasma.
When renin is released into the bloodstream, it acts on angiotensinogen (a circulating layer) that passes through proteolytic cleavage to form decapeptide angiotensin I. Vascular endothelium contains an enzyme called angiotensin transforming enzyme that separates two amino acids and forms -angiotensin II (AII) and other tissues in the body, including the brain and heart, also form angiotensin II (AII).
The components of the renin-angiotensin system are:
- Renin
- Angiotensin I
- Angiotensin II
- Angiotensin-Converting Enzyme (ACE)
Other names for angiotensin
Different types of angiotensin are defined by the Roman numerals, angiotensin IV. Hormones and the way they work are often referred to together as the renin-angiotensin system.
What is angiotensin?
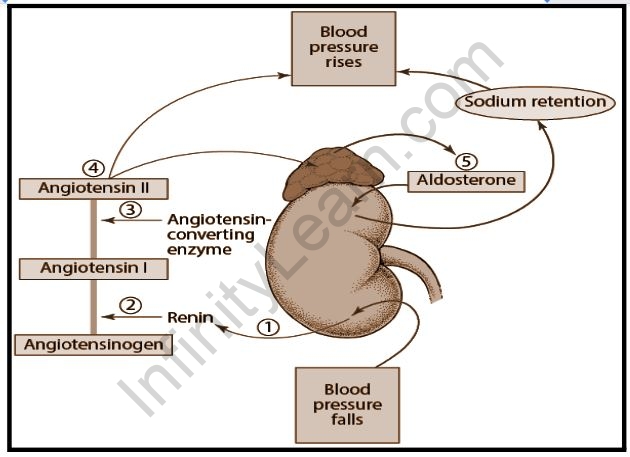
The liver produces and releases a protein called angiotensinogen. This is then broken down by renin, an enzyme produced by the kidneys, to form angiotensin I. This type of hormone is not known to have any biological activity in itself but, rather, is an important precursor to angiotensin II. As it passes through the bloodstream through the lungs and kidneys, it is also metabolized to produce angiotensin II through the action of angiotensin-converting enzymes.
The complete effect of angiotensin II is to increase blood pressure, body fluids, and sodium content. Angiotensin II has effects on:
- Blood vessels: increases blood pressure by causing congestion (narrowing) of blood vessels.
- Sensors: increases the feeling of thirst craving for salt promotes the release of other hormones involved in water retention.
- Adrenal glands: stimulate the production of the hormone aldosterone, which causes the body to retain sodium and lose potassium in the kidneys.
- Kidneys: increase sodium retention and alter the way the kidneys filter blood. This increases the absorption of kidney fluid to increase blood volume and blood pressure.
How is angiotensin administered?
Increased renin production occurs when there is a decrease in sodium levels and a decrease in blood pressure, which is felt by the kidneys. In addition, low blood pressure can stimulate the sympathetic nervous system to increase renin production, leading to increased angiotensinogen conversion to angiotensin I, so the cycle continues.
The renin-angiotensin system is also activated by other hormones, including corticosteroids, estrogen, and thyroid hormones. On the other hand, natriuretic peptides (produced in the heart and central nervous system) can impair the renin-angiotensin system to increase sodium loss in urine.
What happens if I have too much angiotensin?
Excess angiotensin II is a common complication that leads to excess fluid retention by the body and ultimately elevates blood pressure. This usually occurs in heart failure when angiotensin is thought to contribute to the increase in heart size. To combat these side effects, drugs such as angiotensin-converting enzyme inhibitors and angiotensin receptor blockers are used clinically, although these have side effects and can lead to potassium depletion (hyperkalemia).
What happens if I have very low angiotensin?
Regulation of sodium and potassium concentrations in plasma, and control of blood volume and blood pressure, are all hormonal mechanisms that are affected by low levels of angiotensin. Angiotensin deficiency can be associated with potassium depletion, sodium loss, decreased fluid retention (increased urine output), and low blood pressure.
Functions of the Renin-Angiotensin System
Listed below are important functions of the Renin-angiotensin system.
- Build resistant vessels, thereby increasing arterial pressure and systemic vascular resistance.
- It promotes the delivery of sodium to various renal tubular areas and increases water retention in the body.
- It stimulates the release of vasopressin in the posterior pituitary and increases fluid retention by the kidneys.
- It provides the release of norepinephrine into sensitive arteries and prevents norepinephrine absorption, thus enhancing sympathetic adrenergic function.
- It stimulates vascular hypertrophy and cardiac hypertrophy.
- The renin-angiotensin pathway is not only regulated by mechanisms that promote the release of renin but also by the natriuretic peptide released by the human heart, and these peptides serve as an important anti-inflammatory system.
Importance of the Renin-Angiotensin System
The Renin-angiotensin system regulates and maintains blood pressure levels in blood cells. If there is a decrease or increase in blood pressure in a person, this system works faster by releasing renin into the bloodstream.
Deceptive therapies play a major role in treating heart failure and high blood pressure. All receptor blockers and ACE inhibitors are used to reduce arterial blood pressure, blood volume, ventricular congestion, pre-loading ventricular and vascular hypertrophy and reverse cardiac.
Therapies that aim to completely block the Renin-angiotensin system offer additional clinical benefits to patients with kidney and other heart diseases. These methods may include dual inhibition using a combination of Angiotensin II Receptor Blockers and angiotensin-converting enzyme I or therapies such as direct renin inhibition by aliskiren which is a recently approved treatment for hypertension.
Conclusion
Angiotensin is a peptide hormone that causes vasoconstriction and increased blood pressure. It is part of the renin-angiotensin system, which regulates blood pressure. Angiotensin also stimulates the release of aldosterone in the adrenal cortex to promote sodium retention by the kidneys. Angiotensin II is then used to bind all blood vessels. It then increases the maintenance of proper ADH and aldosterone. This stimulates the hypothalamus and activates the thirst reflex. Each reflex leads to an increase in our blood pressure. The main function of the renin enzyme is primarily to cause an increase in blood pressure. This then leads to the restoration of our perfusion pressure which is evident in the kidneys.
Juxtaglomerular kidney cells are responsible for the production of renin, which senses changes in renal perfusion. This is done by the stretch receptors found in our artery walls. These juxtaglomerular cells are also properly stimulated to provide the release of the enzyme renin by rapid signaling from our macula densa.
The main function of the macula densa is to detect certain changes in the delivery of sodium to our distal tubule. It then responds to a sudden decrease in tubular sodium load caused by the stimulation of renin release that occurs in these juxtaglomerular cells. When combined, juxtaglomerular cells and macula densa form the entire juxtaglomerular complex.
Also read: Important Topic of Biology: Renin
FAQs
What effect does angiotensin have on the body?
Angiotensin is a protein hormone that causes blood vessels to become narrower. It helps to maintain blood pressure and fluid balance in the body.
What happens when angiotensin is blocked?
Angiotensin is a chemical in your body that narrows your blood vessels. This narrowing can increase your blood pressure and force your heart to work harder.
What does an increase in angiotensin result in?
Angiotensin II increases blood pressure by stimulating the Gq protein in vascular smooth muscle cells (which in turn activates an IP3-dependent mechanism leading to a rise in intracellular calcium levels and ultimately causing contraction).