Table of Contents
Introduction
The process of Blood Coagulation (Coagulation) is the formation of blood clots. It is an important component of hemostasis, which refers to any process that stops bleeding by forming a clot in the injured arteries. This includes physiological processes in the body as well as pathological processes that lead to uncontrolled bleeding.
Coagulation begins immediately after damage to the blood vessel damages the vessel’s endothelium. The platelets that are normally kept in a state of circulation plasma begin to change the shape, turning it into a circle (called “platelet plug formation”). This starts with Von Willebrand factor (vWF) binding to the subendothelium collagen fibers in the open. VWF changes shape to bind to collagen, and other platelets change shape, forming a small plug that stops bleeding.
The granules in the platelet then release a chemical called Coagulation factor which is responsible for vasoconstriction, thickening at the site of injury. Platelet function is also seen in endothelial cells including the Blood vessel, which releases many smaller packages called platelet alpha granules. These granules contain many aspects of Coagulation that continue to aid in differentiation. In addition, they produce epinephrine that causes additional vasoconstriction at the site of injury.
Blood Cloth Mechanism
The definition of Blood Coagulation states that the process of clotting is a process in which blood clots form, which limits the amount of blood that is lost. This gel-like weight is created from fibrin and platelets. The blood clotting mechanism has various mechanisms that eventually lead to blood clots. Haemostasis (as opposed to bleeding) refers to a process that stops bleeding and helps damaged blood vessels to cool down when the bleeding stops. The Blood Coagulation Method is given below:
The first stage
The Blood Coagulation Machine is known as hemostasis. The first step follows an injury or cut that results in the loss of Blood. This initiates a vasoconstriction process, which causes the walls of the vessels to react more quickly and reduce the amount of blood flowing in the infected region. The first stage is wound healing, in which the Blood begins to form a gel-like substance that can prevent further blood loss.
Second stage
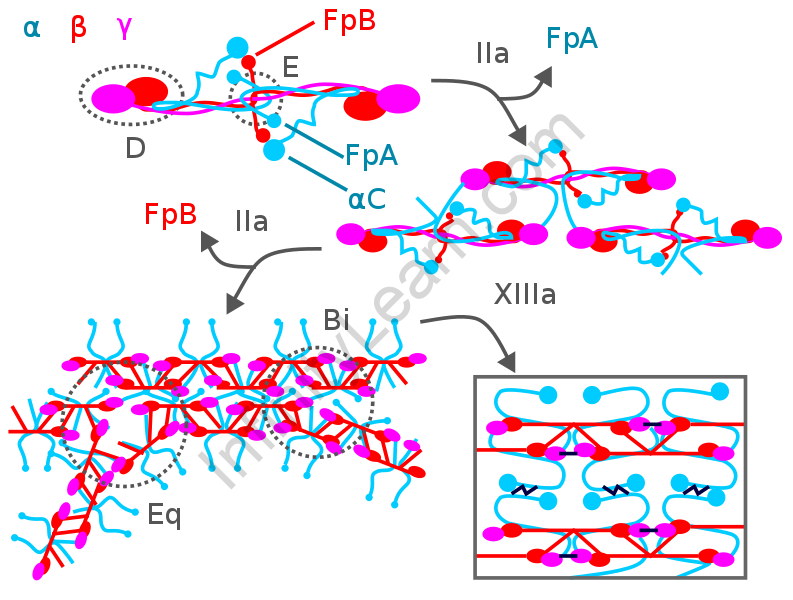
In the second phase of the Blood Coagulation process, platelets play an important role in stopping bleeding in the injured area. This initiates a process called secondary homeostasis which causes the formation of fibrin fibres. The stored granule content includes ADP and thromboxane, which activate platelets within the blood plasma. However, platelets themselves are not enough to completely protect the injured area and form a blood clot. Here are some of the features that keep working and helping each other during a coma.
Third stage
Condensed blood opens the way for the production of fibrinogen, a soluble protein in plasma. Fibrin proteins thicken and form blood clots. If the protein is made up of only platelets, then it is called white thrombosis, and if red blood cells are present, it is called red thrombosis. This is the final step in the process of Blood Coagulation.
Blood Pressure Process
The machine that helps the body to prevent blood loss is often known as hemostasis. The whole process is divided here into three main steps:
Primary hemostasis involves the process of vasoconstriction, which is a response to physical injury to the vascular wall. When damaged, the walls of blood vessels respond quickly by reducing the amount of blood flow to the infected area.
Next, platelets play a key role in covering the injured area to prevent bleeding. They also activate a process that produces a fibrin cell known as secondary hemostasis. This leads to the release of stored granular content containing serotonin, ADP and thromboxane, which leads to the further activation of platelets in blood plasma.
Since platelets alone could not protect against damage to the vessel walls, blood clots should be formed. This formation of blood clots depends on a number of factors that contribute to each other’s thickening.
This flow results in the formation of fibrinogen, a soluble plasma protein. These fibrin proteins eventually bind to the nucleus. Platelet counts are called white thrombus and when red blood cells are present, they are known as red thrombus.
Process of Blood Coagulation
The machine that helps the body to prevent blood loss is often known as hemostasis. The whole process is divided here into three main steps:
Primary hemostasis involves the process of vasoconstriction, which is a response to physical injury to the vascular wall. When damaged, the walls of blood vessels respond quickly by reducing the amount of blood flow to the infected area.
Next, platelets play a key role in covering the injured area to prevent bleeding. They also activate a process that produces a fibrin cell known as secondary hemostasis. This leads to the release of stored granular content containing serotonin, ADP and thromboxane, which leads to the further activation of platelets in blood plasma.
Since platelets alone could not protect against damage to the vessel walls, blood clots should be formed. This formation of blood clots depends on a number of factors that contribute to each other’s thickening.
This flow results in the formation of fibrinogen, a soluble plasma protein. These fibrin proteins eventually bind to the nucleus. Platelet counts are called a white thrombus and when red blood cells are present, they are known as red thrombus.
The most common fluid in the body that circulates everywhere under high pressure and maintains body function is none other than human blood. But massive blood loss can sometimes lead to death.
Blood Coagulation is the process of making a clot or thrombus to prevent excessive blood loss. It is a gel-like compound made up of platelets and fibre in the blood.
FAQ’s
Explain the Mechanism of Blood Clotting.
Coagulation is initiated immediately after damage to the blood vessels that have damaged the endothelium. Blood is expressed in the subendothelial space. It allows two different processes: platelets change, and the subendothelial tissue factor is expressed in plasma factor VII, which leads to the formation of coagulated fibrin. The plug is formed at the site of injury which leads to primary hemostasis. Secondary hemostasis occurs simultaneously. Blood clotting occurs not only in humans but also in all other mammals and animals. In mammals, blood clotting involves both protein and cell components.
What is Deep Vein Thrombosis?
Deep vein thrombosis refers to a serious condition that occurs when blood clots form in deep veins inside the body. The solid blood becomes a clot called a blood clot. Blood clots form in the arteries usually in the lower leg or thigh but may also be created in other parts of the body. Symptoms of the disease may include swelling of the ankle, leg or foot especially on one side, the calf, the skin area feeling warm, red or green in the affected area and severe pain in the foot or ankle.