Table of Contents
Microscopic Anatomy of Testis and Ovary: The testis, the majority of the testis, and the male organ produce sperm, the male reproductive cell, and androgen is the male hormone. In humans, the testicles are oval-shaped organisms that occur in pairs. The testicles are located inside the scrotal sac and are located behind the penis and in front of the anus. The testicles mean the same as the testicles.
The ovary is a female reproductive organ that contains an egg called the ovum. This flow down the fallopian tube continues into the uterus after release, where sperm may be joined. On one side of the body, there is the ovary (from the Latin ovarium ‘egg, nut’). Hormones that are involved in the menstrual cycle and reproduction are also produced by the ovaries. From the stage of pregnancy to the onset of menopause, the ovary goes through several stages. Because of the hormones they produce, they are often classified as endocrine glands.
Microscopic Anatomy of the testicles
In the Microscopic Anatomy of Testis and Ovary, let us first discuss the anatomy of testicles. The visible structure of each standard testicle weighs 25 grams equivalent to 0.875 ounces, four to five inches (1.6 – 2.0 inches), and two to three inches in diameter. Each testis is covered with a fibrous capsule called the tunica albuginea and is further divided by dividing the fibrous tissue from the tunica albuginea into 200 – 400 shaped pieces or sections. In each case, there are 3 -10 threatening tubes, known as seminiferous tubules, whose function is to produce sperm cells. The distinction between the two tubes and the miniferous tubes meets at the same point, near the anus side of each testicle to form the mediastinum testis.

The testicles contain viral cells, which are divided into mature spermatozoa, Sertoli cells (supporting cells), and Leydig cells (intestines) (also known as testosterone-producing cells). The virus cell migrates to the fetal testicles from the embryonic yolk sac, the Sertoli cell is integrated into the germinal epithelial cells within the seminiferous tube, similar to granulosa cells in the ovary. Leydig cells are found beneath the tunica albuginea, on the septal walls, and between tubes similar to internal cells that produce uterine hormones. Leydig cell structure is abnormal and usually has more than one nucleus. These Leydig cells usually contain droplets of oil, pigment granules, and crystalline structure. These cells vary greatly in numbers and appearance between different animal species and are surrounded by blood, lymphatic arteries, and nerve fibers.
In ancient times the embryonic separation of the gonads that did not care for the testicles or ovaries would be determined by the presence or absence of genes that run on the y chromosome.
-
Spermatogenesis
The seminiferous tubule is another, in which sperm is produced and makes up about 90 percent of the testicular weight. In young males, the tubes are simple and made up of underdeveloped sperm cells called spermatogonia and Sertoli cells. When young males mature the tubes become branches and spermatogonia is transformed into fertile sperm cells and after a series of changes, it is called spermatogenesis. Serboli cells are present in both young and old males to mechanically support and prevent spermatogonia. Spermatogonia in the tubules matures into spermatocytes, in addition, they mature into spermatid and mature into spermatozoa as they enter the central lumen of the seminiferous tubule. Spermatozoa are stored in a seminal vesicle that runs through the epididymis and the sperm canal to secrete sperm with semen.
-
Peeled testicles
It is a condition of testicular torsion, in which a twist of sperm occurs and lowers blood flow to the scrotum. As a result of the condition of the crooked testicles, decreased blood flow causes sudden pain and inflammation. This is most common in men aged 12 – 18, but can occur at any stage of life. In this case, it requires urgent surgery, if treated while the testicles can be saved. For whatever reason, if the blood flow is cut for a long time, the testicles may become so damaged that they may need to be removed.
Interesting Facts About Testicles
- Human testicles mean that the testicles produce about 200 million sperm per day.
- In real human testicles, one testicle is usually smaller than the other.
- The human testicle is an organ in the human body, containing more protein than any other organ.
Microscopic Anatomy of Ovary
The female gonads are called ovaries. Each ovary (parts of the ovary) is white and is located in the ovarian fossa, which runs along the lateral uterine wall. The ovarian fossa appears to be the region in front of the ureter and the inner iliac artery surrounded by the external iliac artery. The scale of this region is approximately 4 cm× 3 cm × 2 cm. The formation of the ovary reveals that the capsule surrounds the ovaries, which have the outer cortex and the inner medulla. The tunica albuginea is a capsule made of dense connective tissue.
- Each menstrual cycle, ovulation occurs in one of the two ovaries, which releases the egg.
- The infundibulopelvic muscle connects part of the uterus near the fallopian tube with the tube, and the ovarian muscle connects the other side of the ovary with the uterus.
- The hilum is one of the other structures and tissues of the ovaries.
The formation of the ovary in a human
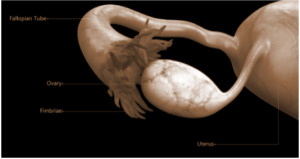
Ligaments: The ovary section indicates that the ovaries are located inside the peritoneal cavity, on both sides of the uterus, and are connected by a fibrous cord known as the ovarian ligament. The ovaries appear in the peritoneal cavity but are attached to the wall of the body by the ovary’s suspensory ligament, which appears to be an extension of the posterior cervical muscle. The mesovarium is the thick layer of the uterus that protects the ovary.
Parts of the fallopian tube, ovarian ligament, mesovarium, and ovarian blood vessels form the ovarian pedicle.
Microanatomy: The germinal epithelium is a membrane that covers the surface of the eggs and is composed of a simple cuboidal-to-columnar mesothelium. The inner structure of the ovary states that the ovarian cortex is the outer layer, made up of ovarian follicles and the stroma in the middle. Cumulus oophorus, membrana granulosa (and granulosa cells within it), zona pellucida, corona radiata, and the main oocyte are all found in the follicle. The follicle usually contains the follicle of the follicle, antrum, and liquor folliculi.
The ovarian medulla is an internal organ. The cortex and medulla are difficult to distinguish, but follicles are rarely found in the medulla.
Follicular cells are flat epithelial cells from the upper epithelium of the ovary. Granulosa cells have shifted from flat to cuboidal and proliferated to form stratified epithelium around them.
Blood vessels and lymphatic vessels are also found in the ovary.
Function
When the girl reaches puberty, the ovary begins to produce more hormones. In response to hormones, secondary sexual characteristics emerge. From imagery, ovary structure, and role change. Because the ovaries have the ability to regulate hormones, these are essential for pregnancy and childbirth. Many reactions activate the endocrine system once the oocytes are released from the Fallopian tube, causing hormonal changes. The hypothalamus and pituitary gland control these responses. The hypothalamus sends messages to the pituitary gland.
The pituitary gland, in addition, releases hormones into the ovaries. The ovaries respond by releasing their hormones in response to this signature.
Gamete Production
The ovaries are where the egg cells, or female gametes, are produced and released regularly. Unripe egg cells (or oocytes) mature in follicles filled with egg fluids. Only one oocyte matures at a time in most cases, but others may mature at the same time.
Follicles are made up of different types and numbers of cells depending on their stage of maturity, and their size indicates the stage of oocyte growth.
Once the oocyte has completed its maturation in the ovary, the pituitary gland produces the luteinizing hormone, which triggers the release of the oocyte through follicle rupture, a process known as ovulation.
Hormone Production
Estrogen, inhibin, androgen, and progestogen are all secreted by mature ovaries. The ovaries contain 50% of testosterone in women until menopause, which is released directly into the bloodstream. The remaining 50% of testosterone in the bloodstream from other parts of the body converts adrenal pre-androgens (DHEA and androstenedione) into testosterone.
Estrogen is responsible for the development of secondary sexual dysfunction in women during puberty, as well as for the maturation and maintenance of fully functional reproductive organs.
Ovarian Aging
Menopause occurs when a woman’s reproductive function decreases as she grows older. A decrease in the number of ovarian follicles is associated with this decrease. Although the human ovary contains about 1 million oocytes at birth, about 500 (approximately 0.05 percent) of these oocytes are ovulated, and the rest are destroyed. Reduction of ovarian reserve usually occurs at a steady rate over the years, with an almost complete reduction of the placenta occurring over the age of 52 years. Pregnancy failure and meiotic defects, result in abnormal chromosomal pregnancies, increased uterine retention and decreased fertility for years.
For about 20-30 years, egg storage and reproduction are high. The menstrual cycle begins to change in about 45 years, and the follicle pool tends to shrink significantly. The causes of ovarian aging are unknown. Environmental factors, life patterns, and genetic factors all play a role in the aging process.
Crack NEET with Result-Oriented Learning Program from Infinity Learn
FAQs
Why Do Some Men Have Three Testicles?
This is due to the rare form of polyorchidism, in which case males are born with more than two testicles. Few of the 200 reported incidents of this nature. Most of them have three testes but also some of them will have more than three testicles. This condition does not have a major health problem but slightly increases the risk of developing testicular cancer.
Question: What Things Can Affect Your Ovaries?
Answer: The things that can affect your ovaries are listed below:
- Ovulation disorders are problems with egg release in the ovaries.
- Polyps or fibroids in the uterus, as well as uterine or cervical anomalies.
- Injury or obstruction of the fallopian tube, which is usually caused by pelvic inflammatory disease.
Infinity Learn App
Now you can find answers to all your subject queries & prepare for your Exams on our Educational App – Infinity Learn.