Table of Contents
Antimicrobial resistance (AMR) occurs when microorganisms, including bacteria, viruses, fungi, and parasites, change in a way that allows them to resist antimicrobial drugs that used to work against them. This resistance can develop through genetic changes or by acquiring resistance genes, making standard treatments ineffective and making infections more difficult to manage.
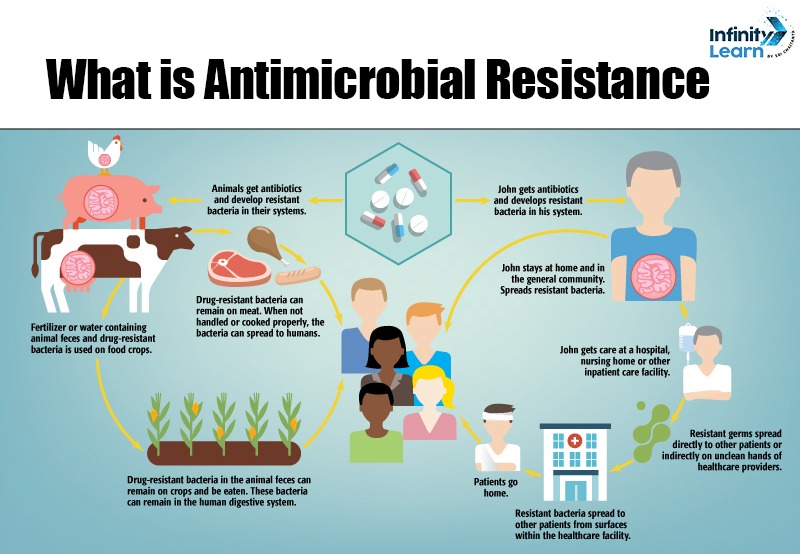
The misuse and overuse of antimicrobial drugs in humans, animals, and agriculture are major factors contributing to AMR. This poses a serious threat to global public health by increasing the risk of disease transmission, severe illness, and death.
Antimicrobial Resistance Definition
Antimicrobial resistance occurs when microorganisms, including bacteria, viruses, fungi, and parasites, develop resistance to antimicrobial medications. As a result, these medicines—such as antibiotics, antivirals, antifungals, and antiparasitics—are no longer effective in treating the infections for which they were intended.
Causes of Antimicrobial Resistance
Antimicrobial resistance (AMR) is a major global health issue caused by several important factors:
- Misuse and Overuse of Antimicrobials: One of the main causes of AMR is the improper use of antibiotics and other antimicrobial drugs. This includes using antibiotics for viral infections, such as the common cold or flu, which they cannot treat, as well as overprescribing antibiotics without appropriate medical advice.
- Agricultural Practices: The use of antibiotics in agriculture, especially in livestock and poultry, to promote growth and prevent disease, significantly contributes to the rise of resistant bacteria. These bacteria can then spread to humans through the food supply.
- Poor Infection Prevention and Control: Insufficient infection control measures in healthcare settings and communities can help resistant bacteria spread. This includes inadequate hygiene practices, poor sanitation, and weak infection control protocols.
- Global Travel and Trade: The movement of people, animals, and goods across borders can facilitate the global spread of resistant bacteria, allowing resistant strains to transfer from one region to another quickly.
- Environmental Factors: Contamination of the environment with antibiotics, such as through waste from pharmaceutical manufacturing or improper disposal of medications, can encourage the development of resistance in environmental bacteria.
- Lack of New Antibiotics: The development of new antibiotics has not kept up with the rise of resistant bacteria. This has created a situation where existing antibiotics are becoming less effective, and few new options are available.
- Genetic Factors: Bacteria can naturally develop resistance through genetic mutations and can also acquire resistance genes from other bacteria through a process called horizontal gene transfer, which allows resistance traits to spread quickly within bacterial populations.
Antimicrobial Resistance Treatment
Antimicrobial resistance (AMR) is a serious global health issue in which microorganisms, such as bacteria, viruses, fungi, and parasites, adapt to resist medications that previously killed them or stopped their growth. This makes infections more difficult to treat and increases the risk of disease spread, severe illness, and death. Treatment Options for Antimicrobial Resistance are as follows:
- Alternative Medications: When standard antibiotics are ineffective, healthcare providers may turn to different classes of antibiotics or use higher doses. For example, carbapenems, such as meropenem, are often effective against resistant bacteria.
- Combination Therapy: Using multiple antibiotics together can sometimes overcome resistance and may be more effective than a single drug.
- Longer Treatment Duration: Extending the length of antibiotic treatment can help eliminate all resistant bacteria.
- Non-Antibiotic Treatments: In certain cases, treatments that do not involve antibiotics, such as phage therapy (which uses bacteriophages to target bacteria) or immunotherapy, can be considered.
- New Antibiotics: Ongoing research and development of new antibiotics are essential. Scientists continuously work to discover and create new drugs to combat resistant strains.
Antimicrobial Resistance Prevention
Antimicrobial resistance (AMR) is a serious global health threat, but there are several strategies to help prevent and control it:
- Responsible Use of Antibiotics: Only use antibiotics when prescribed by a healthcare professional. Do not request antibiotics for viral infections like colds or the flu, as they do not work against viruses.
- Infection Prevention: Practice good hygiene, such as regular handwashing, to prevent infections. Keeping vaccinations up-to-date can also reduce the need for antibiotics.
- Safe Food Handling: Follow food safety guidelines, including cleaning surfaces, separating raw and cooked foods, cooking food thoroughly, and refrigerating leftovers promptly. This helps prevent foodborne illnesses that may require antibiotic treatment.
- Animal Health: Use antibiotics in animals responsibly and only when necessary. This helps minimize the spread of resistant bacteria from animals to humans.
- Public Awareness: Educate yourself and others about the dangers of AMR and the importance of using antibiotics responsibly.
- Global Cooperation: Support policies and initiatives that encourage the responsible use of antibiotics and the development of new treatments.
By following these steps, we can work together to reduce the spread of antimicrobial resistance and protect public health.
Antimicrobial Resistance Control measures
The following are some key measures to control antimicrobial resistance (AMR):
- Prevent Infections: Promote good hygiene practices, vaccination, and infection control measures to reduce the need for antimicrobials.
- Appropriate Use of Antimicrobials: Ensure that antimicrobials are used only when necessary and prescribed correctly.
- Surveillance and Monitoring: Monitor the use of antimicrobials and track resistance patterns to guide policies and practices.
- Education and Awareness: Provide education for healthcare providers, patients, and the public about the risks of AMR and the importance of responsible antimicrobial use.
- Research and Development: Invest in the development of new antibiotics, vaccines, and diagnostic tools.
- Antimicrobial Stewardship Programs: Implement programs in healthcare settings to optimize the use of antimicrobials.
- Global Collaboration: Work with international organizations and countries to address AMR on a global scale.
These measures are essential for effectively managing and reducing the impact of antimicrobial resistance.
Antimicrobial Resistance vs Antibiotic Resistance
Antimicrobial resistance (AMR) and antibiotic resistance are related but different concepts:
Antibiotic Resistance
- Specifically, it refers to bacteria that become resistant to antibiotics, which are drugs meant to kill or stop the growth of bacteria.
- It happens when bacteria mutate or gain resistance genes, making antibiotics less effective or entirely ineffective against them.
Antimicrobial Resistance
- A broader term includes resistance to antibiotics and other types of antimicrobial drugs, such as antivirals, antifungals, and antiparasitics.
- Covers resistance in various microorganisms, including bacteria, viruses, fungi, and parasites.
In summary, while antibiotic resistance is a specific type of antimicrobial resistance, AMR includes a wider range of pathogens and drugs. Both present significant challenges to public health by making infections more difficult to treat.
FAQs on Antimicrobial Resistance
What is antimicrobial resistance?
Antimicrobial resistance (AMR) occurs when microorganisms evolve to resist the effects of drugs that previously eliminated them or inhibited their growth.
What is the use of AMR?
Understanding AMR helps guide treatment options, informs public health strategies, and promotes responsible use of antimicrobials to combat resistant infections.
What are the three types of antimicrobial resistance?
The three types of antimicrobial resistance include resistance to antibiotics, antivirals, and antifungals, affecting various microorganisms
What is the meaning of antibiotic resistance?
Antibiotic resistance specifically refers to bacteria that develop the ability to survive treatment with antibiotics that once effectively killed or inhibited them.