Table of Contents
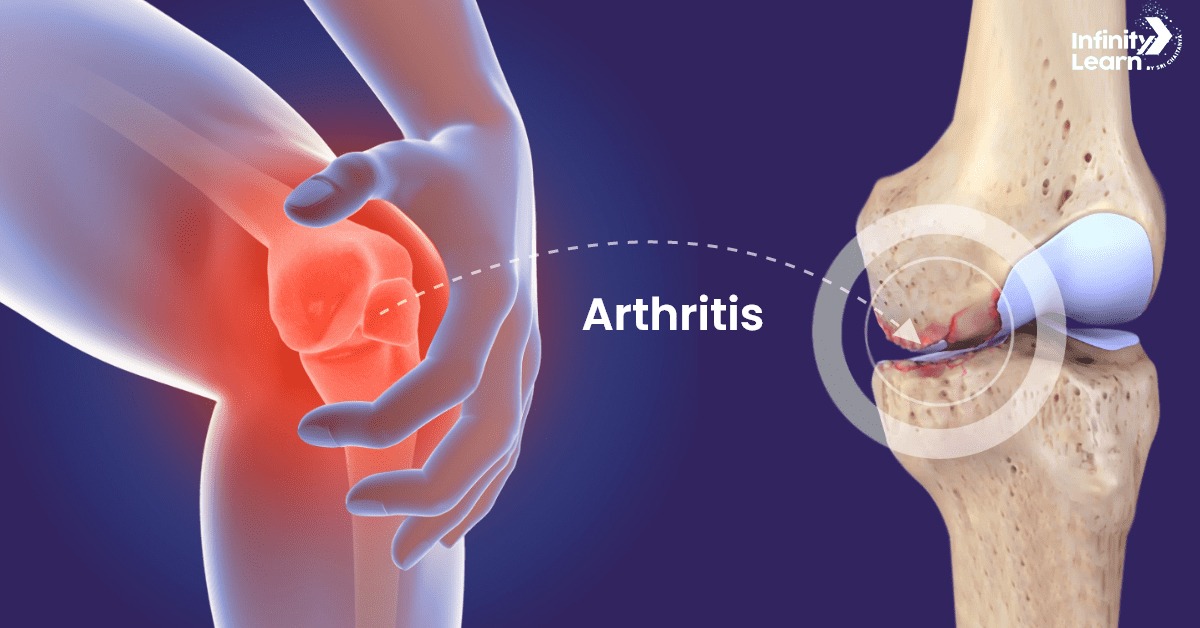
Arthritis Meaning: Arthritis is a general term for inflammation or damage in one or more joints, which are the places where two or more bones connect. When someone has arthritis, the cartilage that protects the ends of the bones can wear away, leading to pain, stiffness, and swelling. There are many types of arthritis, each with different causes and symptoms. The article below explains these types, as well as their symptoms, causes, and treatment options.
Arthritis Types
Arthritis is a general term that includes over 100 different types of joint inflammation and related conditions. The following are some of the most common types:
- Osteoarthritis (OA): The most common type, often called “wear and tear” arthritis. It happens when the cartilage that cushions the bones in the joints slowly breaks down.
- Rheumatoid Arthritis (RA): An autoimmune disease where the immune system attacks the joints, causing inflammation and possible severe damage.
- Psoriatic Arthritis: This type affects some people with psoriasis, a skin condition that causes red patches with silvery scales.
- Gout: Caused by a buildup of uric acid crystals in the joints, leading to sudden, intense pain, redness, and swelling.
- Lupus (Systemic Lupus Erythematosus): A chronic autoimmune disease that can cause inflammation and damage to various body systems, including the joints.
- Ankylosing Spondylitis: Primarily affects the spine but can involve other joints as well. It causes inflammation in the spinal joints, leading to severe, ongoing pain.
- Juvenile Arthritis: Refers to arthritis in children, with juvenile idiopathic arthritis (JIA) being the most common type, causing persistent joint pain, swelling, and stiffness.
Each type of arthritis has its own symptoms and treatment options.
Arthritis Symptoms
Arthritis symptoms can differ depending on the type, but common signs include:
- Joint pain: This can feel like a dull ache or a sharp, burning feeling.
- Stiffness: Often felt more in the morning or after sitting still for a while.
- Swelling: Joints might look bigger than usual and feel warm when touched.
- Redness: The skin around the joint can appear red.
- Decreased range of motion: It can be hard to move the joint fully.
- Tenderness: Joints may feel sensitive to touch.
- Fatigue: Many people with arthritis feel very tired.
- Fever: Sometimes, arthritis can lead to a fever.
Arthritis Causes
Arthritis is a condition that causes inflammation and tenderness in one or more joints. The causes of arthritis can differ based on the type, but some common ones include:
- Wear and Tear: In osteoarthritis, joint cartilage breaks down over time.
- Autoimmune Disorders: In rheumatoid arthritis, the immune system attacks the body’s tissues.
- Infections: Bacterial or viral infections can trigger arthritis.
- Metabolic Issues: Conditions like gout result from high levels of uric acid.
- Injuries: Past joint injuries can lead to arthritis later in life.
- Genetics: A family history of arthritis can increase the risk.
- Obesity: Extra weight stresses joints, especially in the knees, hips, and spine.
Arthritis Risk Factors
Arthritis is a condition that causes joint pain and inflammation. Several factors can increase the risk of developing arthritis:
- Age: The risk of types like osteoarthritis and rheumatoid arthritis increases as people get older.
- Gender: Women are more likely to develop rheumatoid arthritis and osteoarthritis, while men are more prone to gout.
- Family History: Having a family member with arthritis can raise the risk, as some types are hereditary.
- Obesity: Carrying excess weight adds stress to joints, especially in the knees, hips, and spine, increasing the risk.
- Previous Joint Injuries: Injuries from sports or accidents can lead to arthritis in those joints later in life.
- Infections: Certain infections can cause inflammation in the joints.
- Smoking: Smoking is linked to a higher risk of rheumatoid arthritis and can worsen symptoms.
To reduce the risk of developing arthritis, it’s important to maintain a healthy weight, stay active, and avoid joint injuries.
Arthritis Treatment
Arthritis treatment depends on the type and severity of the condition. Here’s a simple overview of common treatments:
- Lifestyle Changes
- Exercise: Regular activity helps keep joints functioning and reduces stiffness. Include strengthening, aerobic, and flexibility exercises.
- Weight Management: Keeping a healthy weight lessens stress on weight-bearing joints, especially knees and hips.
- Medications
- Pain Relievers: Over-the-counter options like paracetamol can help manage pain.
- NSAIDs: Non-steroidal anti-inflammatory drugs, such as ibuprofen and naproxen, reduce pain and inflammation.
- Corticosteroids: These can be taken by mouth or injected to lower inflammation.
- DMARDs: Disease-modifying anti-rheumatic drugs are used mainly for rheumatoid arthritis to slow its progression.
- Supportive Therapies
- Physical Therapy: Improves joint function and muscle strength.
- Occupational Therapy: Teaches how to do daily tasks without stressing the joints.
- Assistive Devices: Tools like canes and walkers can help reduce strain on joints.
- Surgical Options
- Joint Repair: Smoothing or realigning joint surfaces to relieve pain and improve function.
- Joint Replacement: Replacing a damaged joint with an artificial one, often for hips and knees.
- Joint Fusion: Fusing two bones together to stabilize the joint and reduce pain.
- Alternative Treatments
- Acupuncture: Some find relief through acupuncture, which involves inserting thin needles into specific points on the body.
- Supplements: Glucosamine and chondroitin are sometimes used, but their effectiveness is debated.
- Self-Care and Home Remedies
- Hot and Cold Therapy: Heat can relax muscles and relieve pain, while cold can reduce inflammation.
- Rest: Balancing activity with rest is important to avoid stressing the joints.
- Dietary Changes
- Anti-Inflammatory Diet: Eating foods rich in omega-3 fatty acids, antioxidants, and fiber can help reduce inflammation.
Each treatment plan should be customized based on individual needs and medical history, so consulting healthcare professionals is important to find the best approach.
FAQs on Arthritis
What is the main cause of arthritis?
Arthritis is mainly caused by the wear and tear of cartilage in the joints, autoimmune diseases, infections, or metabolic issues
What is the fastest way to treat arthritis?
The quickest way to manage arthritis includes a mix of medications (such as NSAIDs), physical therapy, and lifestyle changes like regular exercise and maintaining a healthy weight.
How to care for arthritis?
Caring for arthritis involves staying active, keeping a healthy weight, eating a balanced diet, using hot and cold packs, and following the treatment plan provided by your doctor.
What age does arthritis start?
Arthritis can begin at any age, but osteoarthritis usually starts after age 50, while rheumatoid arthritis often begins between ages 30 and 60.
Can arthritis be cured?
There is no cure for arthritis, but treatments such as medications, physical therapy, and sometimes surgery can help manage symptoms and improve quality of life.
Is arthritis serious?
Yes, arthritis can be serious as it may lead to chronic pain, joint damage, and reduced mobility if not managed properly.