Table of Contents
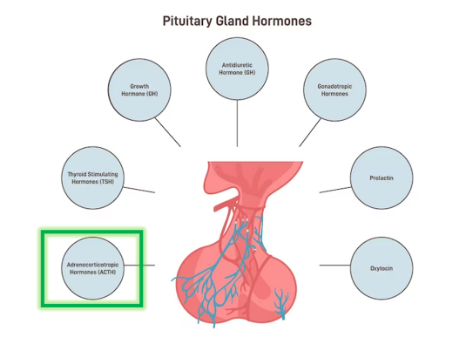
Hormones from the anterior pituitary are produced by five distinct cell types—somatotrophs, thyrotrophs, gonadotrophs, lactotrophs, and corticotrophs—each releasing a specific set of seven hormones. ACTH represents a segment within the larger glycoprotein prohormone molecule known as proopiomelanocortin (POMC). This prohormone is produced by the corticotrophs found in the anterior pituitary, constituting approximately 10 percent of this gland.
Upon secretion from the corticotrophs’ granules, the proopiomelanocortin molecule is cleaved into multiple biologically active polypeptides. Notably, among these polypeptides is ACTH, which primarily triggers the growth and secretion of adrenal cortex cells. Additionally, this hormone contributes to an increase in skin pigmentation. POMC-derived polypeptides also encompass melanocyte-stimulating hormones (alpha- and beta-melanotropin), responsible for heightened skin pigmentation; beta-lipotropin, which prompts the release of fatty acids from adipose tissue; a smaller ACTH fragment, believed to enhance memory; and beta-endorphin, a pain-suppressing agent.
ACTH
Adrenocorticotropic Hormone (ACTH) is a peptide hormone with 39 amino acids. It is predominantly synthesized and secreted by the cells of the anterior pituitary gland, corticotrophs. It reaches the effector organ, the adrenal cortex (outer layer of the adrenal gland) through the peripheral circulation. It plays a pivotal role in the generation and release of cortisol and other essential glucocorticoids by the adrenal gland’s cortex. The secretion of ACTH is under the influence of corticotropin-releasing hormone (CRH), produced by the hypothalamus. This interplay ensures the control of cortisol production.
Various stress-related stimuli, such as instances of low blood glucose or physical trauma, along with interleukin-1 (produced by macrophages) serve as additional triggers for the release of ACTH.
Glucocorticoids, including cortisol, exhibit the ability to inhibit the release of both CRH and ACTH through a negative feedback mechanism. This regulation helps prevent excessive secretion of these hormones, sustaining a delicate equilibrium within the endocrine system.
Negative feedback mechanism
ACTH is involved in a self-regulating loop. serves as the trigger, propelling the adrenal gland’s cortex to release vital glucocorticoids, primarily cortisol. Elevated levels of cortisol in the bloodstream leads to a reduction in the secretion of both ACTH (corticotropin) and corticotropin-releasing hormone (CRH). This effect emerges from cortisol’s ability to suppress the activity of the anterior pituitary corticotrophs and the hypothalamic neurosecretory cells. In this way, the negative feedback mechanism helps maintain an equilibrium within the endocrine system, preventing excessive hormone release and ensuring optimal hormonal balance.
Fluctuations in cortisol levels are typically inversely proportional to changes in ACTH levels. A rise in cortisol levels usually corresponds to a decrease in ACTH levels, while a decrease in cortisol levels typically leads to an increase in ACTH levels.
Both ACTH and cortisol levels follow a daily pattern of variation. ACTH reaches its peak during the early morning hours (around 6 a.m. to 8 a.m.) and reaches its lowest point in the evening (between 6 p.m. and 11 p.m.).
Functions of ACTH
The primary role of adrenocorticotropic hormone (ACTH) is to stimulate the adrenal glands to release cortisol. Cortisol, often referred to as the “stress hormone,” serves a crucial function throughout the body beyond its role in the stress response. Furthermore, ACTH not only triggers the release of cortisol but also stimulates the adrenal glands to release androgens, which are sex hormones. Additionally, ACTH prompts the production of chemical substances that encourage the release of other hormones like adrenaline and noradrenaline, which have significant impacts on various bodily functions.
- Stimulation of spermatogenesis in men: In males, ACTH can stimulate the process of spermatogenesis, which is the production of sperm.
- Stimulation of Dehydroepiandrosterone (DHEA) production: ACTH has a role in promoting the production of DHEA, a precursor to various sex hormones.
- Stimulation of bone resorption: ACTH can contribute to bone resorption by affecting bone turnover, potentially leading to a release of calcium into the bloodstream.
- Catabolism of proteins: ACTH’s actions can result in the breakdown of proteins, which can release amino acids and provide energy during times of stress.
- Metabolic effects: ACTH influences various metabolic processes, including glucose metabolism, androgen production, lipolysis (the breakdown of fats), and the potential for inducing hyperglycemia (high blood sugar levels). It can also suppress the immune system’s response.
- Anabolic Effects on Muscle and bones: Contrary to its catabolic effects, ACTH can also exert anabolic effects on muscle and bone tissues, promoting their growth and maintenance.
Role of ACTH in parturition
The commencement of labor is caused due to complex interplay of both foetal and placental hormones. One critical player in this process is adrenocorticotropic hormone (ACTH). It prompts the foetal adrenal gland to release cortisol and dehydroepiandrosterone (DHEA). Notably, DHEA, under the influence of the placenta, is converted into oestrogen. The surge in oestrogen levels increases the number of receptors for oxytocin on uterine muscle fibres. Oxytocin, released from the posterior pituitary, triggers uterine contractions. Uterine contractions mimic waves, initiating from the top of the uterus and progressing downward, eventually facilitating the expulsion of the foetus.
Disorders of ACTH hormone
- Cushing’s disease: This disorder occurs due to excessive ACTH. It leads to increased cortisol levels, which can result in a range of symptoms including weight gain, high blood pressure, and more.
- Congenital adrenal hyperplasia: Some forms of congenital adrenal hyperplasia can result in abnormal ACTH regulation and adrenal gland function, causing imbalances in hormone production.
- Pituitary tumors: Pituitary tumors can lead to excessive ACTH production, causing conditions like Cushing’s disease or overproduction of other hormones.
- Adrenal insufficiency, including Addison’s disease: Insufficient ACTH production, often due to issues with the pituitary or adrenal glands, can lead to adrenal insufficiency. Addison’s disease specifically refers to primary adrenal insufficiency, where the adrenal glands do not produce enough cortisol and other hormones.
- It’s important to note that ACTH is a key regulator of the body’s stress response and various metabolic processes, and disruptions in its production or function can lead to significant health issues.
Summary
The anterior pituitary gland comprises distinct cell types, each releasing specific hormones. Among them, adrenocorticotropic hormone (ACTH) originates from corticotrophs and is a segment of the larger prohormone proopiomelanocortin. ACTH plays a pivotal role in stimulating adrenal cortex cell growth, cortisol release, and impacting metabolic processes. It follows a negative feedback loop influenced by corticotropin-releasing hormone (CRH) and cortisol. ACTH’s functions include promoting spermatogenesis, influencing dehydroepiandrosterone (DHEA) production, affecting bone resorption, protein catabolism, metabolic processes, and muscle/bone growth. Disorders involve excessive production (Cushing’s disease, pituitary tumors) or insufficient production (adrenal insufficiency, Addison’s disease) of ACTH, underscoring its central role in physiological balance.
FAQs on ACTH Hormones
What is ACTH and where is it produced
ACTH stands for adrenocorticotropic hormone, a peptide hormone produced by the corticotroph cells of the anterior pituitary gland.
What are the functions of ACTH?
ACTH has various functions, including stimulating the growth and secretion of adrenal cortex cells, promoting spermatogenesis in men, influencing the production of dehydroepiandrosterone (DHEA), affecting bone resorption, protein catabolism, metabolic processes, and anabolic effects on muscle and bones.
How is ACTH secretion regulated?
The secretion of ACTH is regulated by corticotropin-releasing hormone (CRH) from the hypothalamus. It follows a negative feedback loop, where elevated levels of cortisol in the bloodstream inhibit the release of both ACTH and CRH to maintain hormonal balance.
What role does ACTH play in childbirth?
ACTH triggers the fetal adrenal gland to release cortisol and dehydroepiandrosterone (DHEA) during childbirth. DHEA is converted to estrogen, leading to increased uterine contractions and the initiation of labor.
What are the disorders related to ACTH?
Disorders involving ACTH include conditions where there is excessive production (Cushing's disease, pituitary tumors) or insufficient production (adrenal insufficiency, Addison's disease). These conditions can lead to hormonal imbalances and various health issues.
How does ACTH interact with cortisol in the body?
ACTH plays a role in regulating cortisol production. Elevated cortisol levels in the bloodstream lead to a reduction in the secretion of both ACTH and corticotropin-releasing hormone (CRH) through a negative feedback mechanism, maintaining hormonal equilibrium.
What other hormones are derived from the same prohormone as ACTH?
The prohormone proopiomelanocortin (POMC), from which ACTH is derived, also produces other hormones like melanocyte-stimulating hormones (alpha- and beta-melanotropin), beta-lipotropin, a smaller ACTH fragment thought to enhance memory, and beta-endorphin, which acts as a pain suppressant.
When are ACTH levels highest during the day?
ACTH levels are highest in the early morning, typically between 6 a.m. and 8 a.m., and lowest in the evening, usually between 6 p.m. and 11 p.m.
How does ACTH impact bone health?
ACTH can influence bone health by promoting bone resorption, affecting bone turnover, and potentially releasing calcium into the bloodstream.