Table of Contents
Heart possesses autorhythmic fibers that allow it to beat spontaneously, its functionality is influenced by processes taking place throughout the body. To sustain health and life, body cells require a specific quantity of oxygen delivered by the bloodstream every minute. When cells are engaged in metabolic activities, such as during exercise, their demand for oxygen from the blood increases. Conversely, during periods of rest, the metabolic requirements of cells decrease, resulting in a reduced workload for the heart.
Cardiac Output
Cardiac output (CO) refers to the quantity of blood expelled from the left or right ventricle into the aorta or pulmonary trunk each minute. It is calculated by multiplying the stroke volume (SV), the blood volume ejected by the ventricle during each contraction, by the heart rate (HR), which denotes the number of heartbeats per minute:
CO (mL/min) = SV (mL/beat) × HR (beats/min)
In an average resting adult male, the stroke volume typically averages 70 mL per beat, and the heart rate is approximately 72 beats per minute. Consequently, the average cardiac output is as follows:
CO = 70 mL/beat × 72 beats/min
= 5040 mL/min
= 5 L/min
This volume is nearly equivalent to the total blood volume, which is around 5 liters in a typical adult male. Therefore, the entire blood volume circulates through the pulmonary and systemic circulations each minute.
Factors influencing cardiac output
Cardiac output is a parameter that is influenced by several factors. Changes in stroke volume or heart rate, lead to changes in cardiac output.
- Stroke Volume (SV): Stroke volume can be influenced by factors such as exercise intensity. During mild exercise, stroke volume may increase, potentially reaching 100 mL per beat, while heart rate simultaneously rises to around 100 beats per minute. This combination results in a substantial increase in cardiac output. In scenarios involving intense but submaximal exercise, heart rate may soar to 150 beats per minute, with stroke volume peaking at 130 mL per beat. These adaptations translate into a remarkable cardiac output of 19.5 L/min, exemplifying the heart’s ability to meet elevated oxygen demands during strenuous physical activity.
- Cardiac Reserve: Cardiac reserve, a critical concept in cardiovascular physiology, refers to the difference between an individual’s maximum achievable cardiac output and their cardiac output at rest. The average person generally possesses a cardiac reserve that is four to five times their resting cardiac output. However, elite endurance athletes, conditioned by rigorous training, may boast a cardiac reserve as high as seven to eight times their resting cardiac output. In contrast, individuals afflicted with severe heart disease may exhibit minimal or negligible cardiac reserve, severely limiting their ability to engage in even routine daily activities.
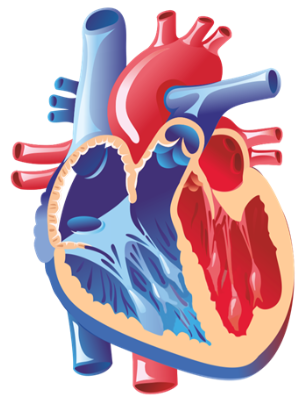
Regulation of Stroke Volume
Stroke volume, a vital factor influencing cardiac output, is precisely regulated by three key components to ensure both ventricles eject equal blood volumes:
- Preload: This term describes heart muscle stretch just before contraction, similar to stretching a rubber band. More stretch means more forceful contractions.
- Contractility: It signifies the strength of ventricular muscle contractions. Enhanced contractility leads to increased stroke volume.
- Afterload: Afterload represents the pressure needed for blood ejection from the ventricles. Elevated afterload makes the heart work harder, potentially reducing stroke volume.
Frank-Starling Law
This law explains how the heart adjusts stroke volume to match blood entering its chambers during relaxation (diastole). It ensures equal blood expulsion from both ventricles, maintaining circulation in both circulatory circuits.
Preload and End-Diastolic Volume (EDV): Preload depends on heart muscle stretch before contraction, linked to EDV, which signifies ventricular blood volume at diastole’s end. More blood during diastole results in stronger contractions during systole.
Factors influencing EDV:
- Duration of Ventricular Diastole: Longer diastolic phases allow more ventricular filling, resulting in larger EDV.
- Venous Return: Increased venous return adds to ventricular blood volume, augmenting EDV.
Balancing ventricular output: The law ensures both ventricles expel equal volumes, maintaining a balance between circulatory circuits. If one side pumps more, increased venous return amplifies EDV in the other ventricle.
Myocardial Contractility
Myocardial contractility, the strength of heart contraction at a given preload, is the second determinant of stroke volume. Positive inotropic agents enhance it, while negative inotropic agents reduce it. Positive agents often boost calcium ion influx during cardiac action potentials, strengthening contractions. Factors affecting contractility include:
- Sympathetic stimulation: Sympathetic nervous system activation intensifies contractility through neurotransmitters like norepinephrine and epinephrine.
- Hormones: Stress or excitement can heighten contractility through hormones like epinephrine and norepinephrine.
- Increased calcium levels: Elevated calcium ions lead to increased contractility.
- Positive inotropic drugs: Certain drugs, like digitalis, have positive inotropic effects.
Negative inotropic effects weaken contractions due to factors like:
- Sympathetic inhibition: Reduced sympathetic activity decreases contractility.
- Anoxia: Lack of oxygen can compromise contractility.
- Acidosis: An acidic environment reduces contractility.
Regulation of Heart Rate
The control of heart rate is a complex process guided by the autonomic nervous system (ANS) and hormones, centered in the medulla oblongata within the brainstem’s cardiovascular center. This center receives inputs from various sources and manages nerve impulses in both the sympathetic and parasympathetic ANS branches.
Autonomic Regulation
- Sympathetic stimulation: Nerves from the medulla to the heart release norepinephrine, which speeds up heart rate and strengthens contractions.
- Parasympathetic stimulation: Vagal nerves slow down heart rate by releasing acetylcholine, primarily affecting the atria.
These systems work together to finely adjust heart rate based on physiological needs and external factors, maintaining cardiovascular stability.
Chemical Regulation
- Hormones: Epinephrine, norepinephrine, and thyroid hormones influence heart rate and contractility, with stress or excitement triggering their release.
- Cations (Ions): Potassium, sodium, and calcium concentrations affect heart rate and contractility, with imbalances potentially causing changes in heart function.
Summary
The heart’s spontaneous rhythm is influenced by various factors to meet the body’s oxygen demands. Cardiac output (CO), the volume of blood ejected by a ventricle per minute, is determined by stroke volume (SV) and heart rate (HR). It typically equals 5 liters per minute, mirroring the body’s total blood volume. SV and HR are regulated to adapt to different conditions. Stroke volume can increase with exercise intensity, demonstrating the heart’s ability to meet oxygen demands during strenuous activity. The cardiac reserve represents the difference between maximum and resting cardiac output, varying among individuals. The Frank-Starling law ensures balanced ventricular blood expulsion, considering preload (stretch), contractility (strength), and afterload (pressure). Myocardial contractility, the strength of contractions at a given preload, is influenced by various factors, including sympathetic stimulation and hormones. Heart rate regulation involves the autonomic nervous system and hormones like epinephrine, ensuring cardiovascular stability.
Numerical Questions
Q1. What will be the stroke volume of a person with 6000 ml of cardiac output and 0.8 sec for each cardiac cycle?
Stroke volume = Cardiac output × Number of beats per minute
Time per each cycle = 0.8 sec
Number of beats per minute = 60/0.8=75beats
Stroke volume = 6000/75=80 ml
Q2. What would be the heart rate of a person if the cardiac output is 5 L blood volume in the ventricles at the end of diastole is 100 mL and at the end of ventricular systole is 50mL?
CO = HR x (EDV – ESV) (Cardiac Output = Heart rate x stroke volume; stroke volume = End Diastole volume – End Systole volume);
We have, CO = 5 Liters, 5000 ml
EDV = 100 ml; ESV = 50 ml
Hence, CO = HR x (EDV – ESV)
HR = CO/(EDV – ESV)
HR = 5000/(100 – 50) = 5000/50
HR = 100bpm
FAQs on Cardiac Output
What is cardiac output, and how is it calculated?
Cardiac output (CO) is the volume of blood ejected by a ventricle of the heart in one minute. It is calculated by multiplying stroke volume (SV), the amount of blood pumped out with each heartbeat, by heart rate (HR), the number of heartbeats per minute. CO = SV × HR.
How does the body regulate cardiac output?
Cardiac output is regulated by adjusting both stroke volume and heart rate. Changes in factors like exercise intensity can influence stroke volume, while the autonomic nervous system and hormones control heart rate to meet the body's oxygen demands.
What is the Frank-Starling law of the heart, and how does it relate to cardiac output?
The Frank-Starling law explains how the heart adjusts its stroke volume to match the volume of blood entering its chambers during relaxation (diastole). It ensures that both ventricles eject equal blood volumes, maintaining balance between the circulatory circuits and contributing to cardiac output regulation.
What factors influence stroke volume, and how do they impact cardiac output?
Stroke volume can be influenced by factors such as exercise intensity. During exercise, stroke volume may increase, leading to a higher cardiac output. Factors affecting stroke volume include preload (stretch), contractility (strength), and afterload (pressure).
How is myocardial contractility related to cardiac output regulation?
Myocardial contractility represents the strength of the heart's contractions at a given preload. It is the second determinant of stroke volume. Positive inotropic factors, like sympathetic stimulation and certain hormones, can enhance contractility, leading to increased stroke volume and cardiac output.
How does the autonomic nervous system regulate heart rate?
The autonomic nervous system (ANS) regulates heart rate through sympathetic and parasympathetic branches. Sympathetic stimulation, mediated by norepinephrine, speeds up heart rate and strengthens contractions. Parasympathetic stimulation, via acetylcholine release, slows down heart rate primarily by affecting the atria.
What role do hormones play in heart rate regulation?
Hormones like epinephrine, norepinephrine, and thyroid hormones influence heart rate and contractility. They are released in response to stress, excitement, or other factors, affecting the heart's rate and strength of contractions.
How can imbalances in cations (ions) like potassium, sodium, and calcium affect heart rate and cardiac function?
Imbalances in cations can have significant effects on heart rate and contractility. Elevated potassium levels can reduce heart rate and contractility, while excess sodium can inhibit calcium influx, weakening contractions and decreasing heart rate. Increased calcium levels can lead to a faster heart rate and stronger contractions.
What is cardiac reserve, and why is it important?
Cardiac reserve is the difference between an individual's maximum achievable cardiac output and their cardiac output at rest. It varies among individuals and can be influenced by factors like fitness level. It is crucial because it reflects the heart's ability to respond to increased oxygen demands during exercise or stress.