Table of Contents
Coronary Artery Disease (CAD) is a significant medical issue, impacting approximately 7 million individuals annually. The development of CAD is attributed to the gradual buildup of plaques within the coronary arteries, ultimately leading to a decreased blood supply to the heart muscle. While certain individuals remain asymptomatic, others encounter symptoms such as angina pectoris (chest pain), and a portion of them even face the ordeal of heart attacks.
Risk Factors
Risk factors for CAD include smoking, elevated blood pressure, diabetes, high levels of cholesterol, obesity, possessing a “type A” personality, leading a sedentary lifestyle, and having a family history of CAD. Many of these factors can be altered by adjusting dietary and lifestyle habits or managed through medications. However, some factors remain unmodifiable, lying beyond our influence. These unchangeable factors encompass genetic predisposition (a familial history of CAD at an early age), advancing age, and gender. Notably, adult males have a higher predisposition to CAD compared to adult females; this discrepancy levels out around the age of 70. Smoking, undeniably, holds the top position among all CAD-related risk factors, approximately doubling the risk of both morbidity and mortality associated with the condition.
Formation of Plaques
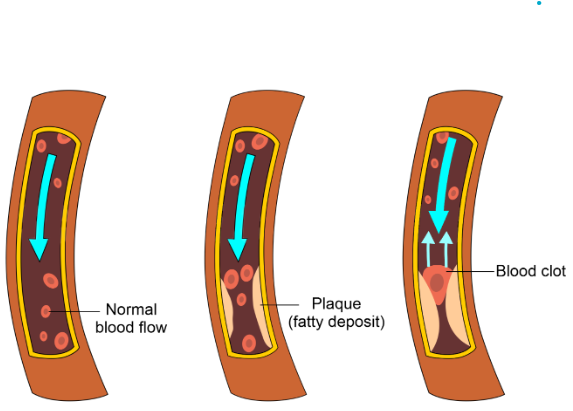
Arteriosclerosis, a group of diseases characterized by the thickening of artery walls and loss of elasticity, includes atherosclerosis, a progressive ailment marked by the development of atherosclerotic plaques within the walls of large and medium-sized arteries.
Lipoproteins are the molecules produced by the liver and small intestine. These spherical entities consist of a central core of triglycerides and other lipids enveloped by proteins, phospholipids, and cholesterol. Cholesterol, being hydrophobic, necessitates rendering it water-soluble for transportation through the bloodstream. This is achieved by coupling it with lipoproteins, where two key types are low-density lipoproteins (LDLs) and high-density lipoproteins (HDLs). LDLs transport the cholesterol from the liver to body cells for membrane repair, steroid hormone production, and bile salt synthesis. However, excessive LDL levels foster atherosclerosis, labeling the cholesterol within as “bad cholesterol.” Conversely, HDLs eliminate surplus cholesterol from cells and transport it to the liver for disposal. As HDLs reduce blood cholesterol, the cholesterol they carry is referred to as “good cholesterol.” Ideally, one aims for low LDL levels and high HDL levels.
Inflammation, the body’s protective response to tissue damage, is pivotal in atherosclerotic plaque development. Tissue damage prompts blood vessels to dilate, enhance permeability, and recruit phagocytes, including macrophages. The genesis of atherosclerotic plaques commences with the accumulation of excess LDLs within the inner artery wall layer (nearest the bloodstream). Here, the lipids and proteins within LDLs undergo oxidation and protein binding to sugars. This triggers the artery’s endothelial and smooth muscle cells to release substances attracting monocytes from the blood, which are then transformed into macrophages. These macrophages consume oxidized LDL particles to become “foam cells.” T cells subsequently infiltrate the artery’s inner lining, releasing chemicals that amplify the inflammatory response. Foam cells, macrophages, and T cells collaborate to form a fatty streak, the initial stage of an atherosclerotic plaque.
Macrophages secrete compounds that induce smooth muscle cells in the artery’s middle layer to migrate atop the atherosclerotic plaque, creating a cap that isolates it from the bloodstream. Most atherosclerotic plaques expand outward rather than encroach on the bloodstream, thus allowing blood flow through the affected artery relatively unimpeded, often for decades. Heart attacks are less frequently triggered when plaque in a coronary artery extends into the bloodstream, narrowing blood flow. More commonly, heart attacks occur when the plaque’s cap ruptures in response to chemicals produced by foam cells. Additionally, T cells prompt foam cells to produce tissue factor (TF), initiating a sequence of reactions culminating in blood clot formation. If a clot within a coronary artery becomes sufficiently large, it can severely diminish or halt blood flow, precipitating a heart attack.
Several other modifiable risk factors also play significant roles in CAD prediction when elevated. C-reactive proteins (CRPs), present in the bloodstream in an inactive state and activated during inflammation, might contribute directly to atherosclerosis by encouraging macrophages to take up LDLs. Lipoprotein (a), resembling LDL, binds to endothelial cells, macrophages, and platelets, potentially spurring smooth muscle fiber proliferation and impeding clot breakdown. Fibrinogen, a glycoprotein involved in clotting, could help regulate cellular growth, vasoconstriction, and platelet aggregation. Homocysteine, an amino acid, might induce blood vessel damage by promoting platelet aggregation and smooth muscle fiber proliferation.
Diagnosis
Electrocardiogram (ECG): This standard test is employed for CAD diagnosis. Stress testing is another option. During exercise stress testing, the heart’s performance under physical strain is monitored through activities like treadmill or exercise bike usage. Continuous ECG readings and blood pressure checks are done. For those who can’t exercise, nonexercise stress tests involve injecting a medication to simulate exercise stress. Radionuclide imaging may be added to evaluate heart muscle blood flow.
- Echocardiography: Using ultrasound waves, echocardiography provides moving images of the heart’s interior. It helps assess chamber sizes, shapes, and functions, blood volume and velocity, heart valve status, birth defects, and pericardium abnormalities.
- Electron Beam Computerized Tomography (EBCT): This method identifies calcium deposits in coronary arteries, indicative of atherosclerosis, providing insights into CAD.
- Coronary (Cardiac) computed tomography radiography (CCTA): By injecting a contrast medium and using x-rays, this procedure creates a CCTA scan image. It’s effective for detecting blockages like atherosclerotic plaques or calcium deposits.
- Cardiac catheterisation: Invasive and versatile, cardiac catheterization visualizes the heart’s chambers, valves, and vessels. It aids in diagnosis and non-coronary disease treatment. Pressure measurements, cardiac output assessment, blood flow measurements, and sample collection are possible. A catheter is inserted via a peripheral vein (right heart catheterization) or artery (left heart catheterisation) under x-ray guidance.
- Coronary angiography: This invasive procedure examines coronary arteries. A catheter inserted into the groin or wrist is guided under X-ray to coronary arteries. A radiopaque contrast medium is injected, and angiograms of the arteries are recorded. This technique can visualize coronary arteries and deliver clot-dissolving drugs directly into them if needed.
In essence, these diagnostic methods offer a range of techniques to effectively identify and assess CAD, enabling appropriate medical intervention.
Treatment
Effective management of CAD encompasses a range of approaches, including medication, surgical interventions, and nonsurgical procedures, all geared toward enhancing blood supply to the heart.
- Medications: CAD treatment involves various drugs, such as antihypertensives, nitroglycerin, beta-blockers, cholesterol-lowering medications, and clot-dissolving agents.
- Coronary Artery Bypass Grafting (CABG): This surgical procedure entails grafting a blood vessel from another body part onto a coronary artery to bypass a blockage. The grafted vessel bridges the aorta and unobstructed segment of the coronary artery. Complex cases might require multiple grafts.
- Percutaneous Transluminal Coronary Angioplasty (PTCA): This non-surgical procedure involves inserting a balloon catheter through an arm or leg artery and guiding it into a coronary artery. Angiograms locate plaques, and a balloon inflates to compress the plaque against the artery wall. Restenosis (re-narrowing) of opened arteries, common in 30-50% of cases within six months, can be mitigated by inserting a stent via catheter. Stents are fine metallic wire tubes permanently placed in arteries to keep them open. Drug-coated stents, containing anti-proliferative and anti-inflammatory drugs, reduce restenosis rates compared to bare-metal stents.

- Laser-Emitting Catheters and Directional Coronary Atherectomy: Laser-based catheters vaporise plaques (excimer laser coronary angioplasty or ELCA), while blade-equipped catheters remove plaque sections (directional coronary atherectomy).
- Cold Therapy Research: Ongoing studies explore cooling the body’s core temperature during procedures like CABG. Positive outcomes, similar to cases of hypothermic incidents, have been observed after cold therapy application during cerebral vascular accidents (strokes).
Summary
Coronary Artery Disease (CAD) affects millions annually due to the accumulation of atherosclerotic plaques in coronary arteries, leading to reduced blood flow to the heart. Risk factors, including modifiable ones like smoking, hypertension, high cholesterol, and sedentary lifestyles, contribute to its development. Unmodifiable factors, such as genetics, age, and gender, also play roles. Plaque formation is driven by lipoproteins, with LDLs contributing to plaque buildup and HDLs working to eliminate excess cholesterol. Inflammation further exacerbates plaque growth. Diagnostic methods, from ECGs to angiography, enable accurate CAD assessment. Treatment encompasses medications, bypass surgery, angioplasty, and innovative techniques. The goal is to enhance blood supply, mitigating the risk of heart attacks and related complications.
FAQs on Coronary Artery Disease
What is Coronary Artery Disease (CAD)?
Coronary Artery Disease (CAD) is a medical condition characterized by the gradual buildup of atherosclerotic plaques in the coronary arteries, resulting in reduced blood flow to the heart muscle. It can lead to various symptoms and complications, including angina and heart attacks.
What are the risk factors for CAD?
Risk factors for CAD include smoking, high blood pressure, diabetes, elevated cholesterol levels, obesity, sedentary lifestyle, possessing a type A personality, and having a family history of CAD. Some factors can be modified through lifestyle changes or medication, while others, like genetics, age, and gender, are beyond our control.
How do lipoproteins contribute to CAD?
Lipoproteins are molecules produced by the liver and small intestine that transport cholesterol in the bloodstream. Low-density lipoproteins (LDLs) carry cholesterol to cells, but excessive LDL levels can lead to atherosclerosis. High-density lipoproteins (HDLs) remove excess cholesterol from cells, contributing to a healthier cholesterol balance.
How does inflammation play a role in atherosclerotic plaque development?
Inflammation, the body's protective response to tissue damage, is pivotal in the development of atherosclerotic plaques. It prompts blood vessel dilation, increased permeability, and the recruitment of immune cells like macrophages. These cells accumulate oxidized LDL particles, forming foam cells that initiate plaque formation.
What are common diagnostic methods for CAD?
Diagnostic methods for CAD include resting electrocardiograms (ECGs), stress tests, echocardiography (ultrasound imaging of the heart), electron beam computerized tomography (EBCT) to detect calcium deposits, and coronary angiography, which uses contrast dye and x-rays to visualize coronary arteries.
What are the treatment options for CAD?
Treatment for CAD varies and can include medications such as antihypertensives, nitroglycerin, beta blockers, and cholesterol-lowering drugs. Surgical interventions like coronary artery bypass grafting (CABG) involve grafting blood vessels to bypass blockages. Nonsurgical procedures include percutaneous transluminal coronary angioplasty (PTCA) and stent placement to open narrowed arteries.
How can CAD be prevented?
Preventing CAD involves adopting a healthy lifestyle: quitting smoking, maintaining a balanced diet, engaging in regular physical activity, managing blood pressure and cholesterol levels, and controlling diabetes. Regular medical check-ups and adherence to prescribed medications also play vital roles in prevention.
What is the significance of early CAD diagnosis and intervention?
Early diagnosis and intervention are crucial to managing CAD effectively and minimising its impact. Identifying risk factors, undergoing appropriate diagnostic tests, and initiating treatment promptly can reduce the risk of complications like heart attacks, enhance quality of life, and improve long-term outcomes.