Table of Contents
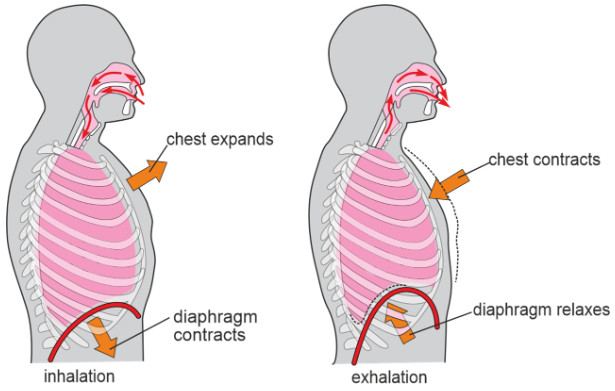
Breathing, or respiration, is a fundamental process that allows organisms to exchange gases with their environment. In mammals, including humans, breathing involves the inhalation of oxygen-rich air and the exhalation of carbon dioxide. This process is essential for supplying oxygen to the body’s cells and removing waste carbon dioxide. The mechanics of inhalation and exhalation are achieved through the coordinated action of various muscles and changes in lung volume.
Inhalation (Inspiration)
- Inhalation, also known as inspiration, is the process of breathing in the air into the lungs. Before each inhalation, the air pressure inside the lungs is equal to the atmospheric pressure at sea level, which is approximately 760 millimeters of mercury (mmHg) or 1 atmosphere (atm). To initiate inhalation, the pressure inside the alveoli (small air sacs in the lungs) must become lower than atmospheric pressure, causing air to flow into the lungs.
- Boyle’s law: The pressure of a gas in a closed container, like the lungs, is inversely proportional to the volume of the container. Boyle’s law describes this relationship, stating that increasing the container’s size decreases the gas’s pressure, and vice versa. When the thoracic cavity expands during inhalation, the volume of the lungs increases, leading to a decrease in the pressure inside the lungs.
- Muscles involved in inhalation: The primary muscle responsible for inhalation is the diaphragm, a dome-shaped skeletal muscle that separates the thoracic and abdominal cavities. Contraction of the diaphragm causes it to flatten, increasing the vertical diameter of the thoracic cavity and expanding the lungs. The external intercostal muscles, located between the ribs, also play a role in inhalation by elevating the ribs, which further increases the chest cavity’s dimensions.
- Intrapleural pressure: The intrapleural pressure, the pressure within the pleural cavity (the space between the visceral and parietal pleura), is always lower than atmospheric pressure. This negative pressure creates a vacuum-like effect that attaches the lungs to the chest wall. As the thoracic cavity expands during inhalation, the volume of the pleural cavity increases, reducing intrapleural pressure even further.
Exhalation (Expiration)
Exhalation, or expiration, is the process of breathing out air from the lungs. During quiet breathing, exhalation is a passive process driven by the elastic recoil of the chest wall and lungs. When the inspiratory muscles relax, the diaphragm moves upward due to its elasticity, and the ribs are depressed, reducing lung volume. This leads to an increase in alveolar pressure, causing air to flow out of the lungs to the lower atmospheric pressure.
- Active Exhalation: Forceful exhalation, as seen during intense exercise or playing wind instruments, involves the active contraction of muscles. The abdominal muscles and internal intercostals are the primary muscles of active exhalation. Contraction of these muscles elevates intra-abdominal pressure and pulls the ribs downward, further reducing lung volume and increasing alveolar pressure, facilitating the expulsion of air.
Respiratory Volumes and Capacities
Lung volumes and capacities, which vary during inhalation and exhalation, depend on factors such as individual characteristics and pulmonary health. These can be categorized into lung volumes, directly measured using a spirometer, and lung capacities, which are combinations of different lung volumes. Spirometry records these variations, with inhalation as an upward deflection and exhalation as a downward one. These measurements vary among individuals based on gender, height, age, altitude, and obesity, and abnormal values can help diagnose respiratory disorders.
Respiratory volumes
Tidal volume (TV)
When at rest, an average healthy adult takes about 12 breaths per minute, each moving around 500 mL of air in and out of the lungs. This inhaled and exhaled volume is termed the tidal volume (TV). Roughly 70% of this volume (350 mL) reaches the respiratory zone, participating in external respiration. The remaining 30% (150 mL) remains in the conducting airways, collectively known as the anatomic dead space, as it doesn’t undergo gas exchange.
Inspiratory reserve volume (IRV)
Beyond the tidal volume, additional inhaled air can be taken during a deep breath. This extra volume, known as the inspiratory reserve volume (IRV), averages around 2500-3000 mL. By forcefully exhaling after a normal inhalation, more air than the tidal volume can be exhaled.
Expiratory reserve volume (ERV)
The forced expiratory volume in 1 second (FEV1) measures the amount of air that can be exhaled within 1 second after a maximal inhalation, and it’s significantly affected by conditions like chronic obstructive pulmonary disease (COPD). It averages around 1000-1100 mL.
Residual volume (RV)
Even after the expiratory reserve volume is exhaled, some air remains due to sub-atmospheric intrapleural pressure, keeping alveoli slightly inflated and maintaining non-collapsible airways. This volume, not measurable by spirometry, is termed the residual volume (RV), which averages about 1100 mL-1200 mL.
Minimal volume (MV)
Opening the thoracic cavity equalizes intrapleural pressure to atmospheric pressure, expelling part of the residual volume. The remaining air is referred to as the minimal volume. This concept holds significance in medical and legal contexts, especially in determining stillbirth or post-birth death. The presence of minimal volume is demonstrated by observing whether a piece of lung floats in water; the absence of air in foetal lungs prevents floating.
Lung Capacities
Lung capacities are vital indicators of respiratory health, combining specific lung volumes to paint a comprehensive picture of pulmonary function. Understanding these capacities provides essential insights into breathing efficiency and overall lung performance. Lung capacities emerge from combinations of distinct lung volumes.
- The inspiratory capacity (IC) is the sum of the tidal volume and inspiratory reserve volume.
- Functional residual capacity (FRC) is determined by adding the residual volume to the expiratory reserve volume.
- Vital capacity (VC) is the aggregation of inspiratory reserve volume, tidal volume, and expiratory reserve volume.
- Total lung capacity (TLC) is the sum of vital capacity and residual volume.
Summary
Breathing, a fundamental physiological process, enables gas exchange in mammals, including humans, by inhaling oxygen-rich air and exhaling carbon dioxide. This process sustains cellular oxygen supply and eliminates waste carbon dioxide. Inhalation involves lowering air pressure in the lungs to draw in air, driven by the diaphragm’s contraction and rib movement due to Boyle’s law. Exhalation, mainly passive, results from elastic recoil, but active exhalation uses muscles like the abdominal and internal intercostals. Respiratory volumes and capacities play a crucial role in lung function assessment; tidal volume moves 500 mL of air with each breath, while inspiratory reserve volume adds extra inhalation capacity, and expiratory reserve volume aids forceful exhalation. Residual volume maintains lung inflation, and minimal volume has forensic implications. Lung capacities, like inspiratory capacity, functional residual capacity, vital capacity, and total lung capacity, provide a holistic view of lung function. Understanding these dynamics is essential for evaluating respiratory health and efficiency.
FAQs on Mechanism of Breathing
What is respiration, and why is it important?
Respiration, or breathing, is the process by which organisms exchange gases with their environment, specifically oxygen and carbon dioxide. In mammals, including humans, respiration is vital for supplying oxygen to cells and removing waste carbon dioxide, essential for cellular metabolism and survival.
How does inhalation work?
Inhalation, also known as inspiration, involves lowering the air pressure within the lungs below atmospheric pressure to draw air in. This process is facilitated by the contraction of the diaphragm and elevation of the ribs, leading to increased lung volume and decreased pressure inside the lungs. Boyle's law explains this inverse relationship between gas pressure and volume.
What is exhalation, and how does it occur?
Exhalation, or expiration, is the process of expelling air from the lungs. During quiet breathing, it's a passive process driven by the elastic recoil of the chest wall and lungs. When inspiratory muscles relax, the diaphragm moves upward, and the ribs are depressed, reducing lung volume. Forceful exhalation involves the active contraction of muscles like the abdominal and internal intercostals, further decreasing lung volume.
What are respiratory volumes and capacities?
Respiratory volumes are different amounts of air moved during specific breathing activities. Tidal volume (TV) is the volume of air moved during normal breathing. Inspiratory reserve volume (IRV) is the extra air that can be inhaled after a deep breath, while expiratory reserve volume (ERV) is the extra air exhaled forcefully after a normal exhalation. Residual volume (RV) is the air that remains in the lungs after maximal exhalation. Minimal volume (MV) is significant in determining stillbirth or post-birth death.
What are lung capacities, and why are they important?
Lung capacities are combinations of specific respiratory volumes that provide a holistic view of lung function. They help evaluate respiratory health and efficiency. Inspiratory capacity (IC) combines tidal volume and inspiratory reserve volume, functional residual capacity (FRC) combines residual volume and expiratory reserve volume, vital capacity (VC) combines inspiratory reserve volume, tidal volume, and expiratory reserve volume, and total lung capacity (TLC) combines vital capacity and residual volume.
How is lung function assessed?
Lung function can be assessed by measuring respiratory volumes and capacities using devices like a spirometer.
What is the role of anatomic dead space in respiration?
Anatomic dead space refers to the portion of inhaled air that doesn't reach the respiratory zone, as it remains in the conducting airways. This air doesn't participate in gas exchange. Anatomic dead space is important in understanding the efficiency of gas exchange in the respiratory system.
Why are lung capacities significant in medical and legal contexts?
Lung capacities are essential in medical assessments to understand respiratory health and diagnose conditions like chronic obstructive pulmonary disease (COPD). In legal contexts, concepts like minimal volume play a role in determining stillbirth or post-birth death.
How do inspiratory and expiratory muscles contribute to breathing?
Inspiratory muscles, primarily the diaphragm and external intercostal muscles, expand the thoracic cavity and increase lung volume during inhalation. Expiratory muscles, such as the internal intercostal muscles and abdominal muscles, aid in active exhalation, especially during intense activities or forceful exhalations.
What is the significance of Boyle's law in respiration?
Boyle's law states that gas pressure is inversely proportional to its volume in a closed container. This principle is crucial in understanding the pressure changes that drive inhalation and exhalation. When the thoracic cavity expands during inhalation, lung volume increases, leading to decreased air pressure inside the lungs and drawing in air.