Table of Contents
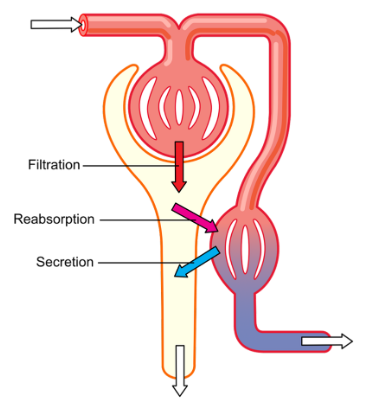
The kidneys play a vital role in maintaining the body’s internal environment by regulating the composition and volume of body fluids. The primary function of the kidneys is the formation of urine, a process that involves three basic steps: Glomerular Filtration, Tubular reabsorption, and Tubular secretion.
Glomerular Filtration
Glomerular filtration is the initial step in urine production, taking place in the renal corpuscles of the kidneys. The renal corpuscles consist of the glomerulus, a tuft of capillaries, and the Bowman’s capsule, a double-walled structure that surrounds the glomerulus.
The filtration membrane consists of three layers: the endothelium of glomerular blood vessels, the epithelium of Bowman’s capsule, and the basement membrane between them. This membrane is permeable to water and small solutes but prevents the filtration of most plasma proteins, blood cells, and platelets, ensuring that only waste products and necessary substances enter the glomerular capsule.
The glomerular endothelial cells have fenestrations or pores, while the basal lamina prevents the filtration of larger negatively charged plasma proteins. The podocytes, which are specialized epithelial cells of Bowman’s capsule, have intricate arrangements that create filtration slits or slit pores, allowing the passage of essential molecules such as water, glucose, amino acids, vitamins, small plasma proteins, ammonia, urea, and ions.
Net Filtration Pressure
Filtration occurs as a result of pressure differences across the filtration membrane. The net filtration pressure (NFP) is the driving force that moves fluid across the membrane. It depends on three main pressures:
- Glomerular Blood Hydrostatic Pressure (GBHP): This is the blood pressure in the glomerular capillaries, promoting filtration by forcing water and solutes in the blood plasma through the filtration membrane. GBHP is approximately 60 mmHg.
- Capsular Hydrostatic Pressure (CHP): CHP opposes filtration and is the hydrostatic pressure exerted by the fluid already present in the capsular space and renal tubule. CHP is around 18 mmHg.
- Blood Colloid Osmotic Pressure (BCOP): BCOP is due to the presence of proteins like albumin, globulins, and fibrinogen in blood plasma, and it also opposes filtration. The average BCOP in glomerular capillaries is about 32 mmHg.
NFP can be calculated by the following formula:
Net Filtration Pressure (NFP) = GBHP – (CHP + BCOP) = 60 mmHg – (18 mmHg + 32 mmHg) = 10 mmHg
Glomerular Filtration Rate (GFR)
The amount of filtrate formed by both kidneys per minute is called the glomerular filtration rate (GFR). GFR is a crucial measure of kidney function. In a healthy adult, the GFR is approximately 125 ml/minute, which amounts to an astounding 180 liters per day. This means that around 1/5th of the blood pumped out by each ventricle of the heart per minute (renal blood flow) is filtered by the kidneys.
After glomerular filtration, the resulting filtrate undergoes further processing through two critical processes: tubular reabsorption and tubular secretion.
Tubular reabsorption
This process involves the movement of substances from the filtrate back into the blood, ensuring that essential nutrients and the majority of electrolytes and water are retained within the body. Nearly 99% of the filtrate, amounting to around 180 litres per day, is reabsorbed by the renal tubules. Different segments of the nephron are responsible for reabsorbing substances actively or passively. For example, glucose, amino acids, and sodium ions are actively reabsorbed, while nitrogenous wastes are absorbed passively. Reabsorption of water also occurs passively in the initial segments of the nephron.
Tubular secretion
In this process, certain substances are actively transported from the blood into the nephron, further modifying the composition of the filtrate. Renal tubule and duct cells secrete substances like hydrogen ions (H+), potassium ions (K+), ammonia, and drugs into the filtrate. Tubular secretion is essential for maintaining the ionic and acid-base balance of body fluids and controlling blood pH.
Role of different nephron segments in reabsorption and secretion
The various segments of the nephron have specific roles in the reabsorption and secretion processes:
- Proximal Convoluted Tubule (PCT): The majority of essential nutrients and 70-80% of electrolytes and water are reabsorbed in the PCT. Active transport of sodium ions drives the reabsorption of other solutes like chloride ions (Cl-) and water, which follow passively due to osmosis. Additionally, selective secretion of hydrogen ions, ammonia, and potassium ions occurs in the PCT.
- Loop of Henle: Reabsorption is minimal in the ascending limb but significant in the descending limb. The descending limb is permeable to water, allowing obligatory water reabsorption by osmosis. In the ascending limb, sodium chloride (NaCl) and potassium ions (K+) are actively reabsorbed, contributing to the maintenance of high osmolarity in the medullary interstitial fluid.
- Distal Convoluted Tubule (DCT): Conditional reabsorption of sodium ions and water occurs in the DCT. It also selectively secretes hydrogen ions (H+), potassium ions (K+), and ammonia to maintain pH and sodium-potassium balance in the blood.
- Collecting Duct: The collecting duct extends from the cortex to the medulla, and large amounts of water can be reabsorbed from this region to produce concentrated urine. The permeability of the medullary collecting duct to water is controlled by antidiuretic hormone (ADH), also known as vasopressin. With high levels of ADH, the collecting duct becomes permeable to water, allowing for facultative water reabsorption and producing concentrated urine. ADH secretion is regulated based on the body’s water needs.
Countercurrent mechanisms
The kidneys employ two countercurrent mechanisms, countercurrent multiplication, and countercurrent exchange, to create and maintain the osmotic gradient in the renal medulla.
Countercurrent multiplication involves the long nephron loops of juxtamedullary nephrons. The osmotic gradient is established through the countercurrent flow of tubular fluid, resulting in a medullary interstitial fluid osmolarity ranging from 300 mOsm/liter in the outer medulla to 1200 mOsm/liter deep in the inner medulla.
Countercurrent exchange occurs in the vasa recta, where blood flows in opposite directions in the ascending and descending parts. This allows for the passive exchange of solutes and water between the blood and interstitial fluid of the medulla without diminishing the osmotic gradient.
Summary
The kidneys form urine through glomerular filtration, tubular reabsorption, and tubular secretion. Glomerular filtration removes waste while retaining essential substances. The net filtration pressure drives this process. The glomerular filtration rate (GFR) measures kidney function. Tubular reabsorption reabsorbs nutrients and water, while tubular secretion eliminates certain substances. Different nephron segments have specific roles in these processes. Countercurrent mechanisms maintain the medullary osmotic gradient.
FAQs on Urine Formation
What are the three basic processes involved in urine formation?
The three basic processes involved in urine formation are glomerular filtration, tubular reabsorption, and tubular secretion.
How does glomerular filtration work?
Glomerular filtration occurs in the renal corpuscles, where the filtration membrane allows water and small solutes to pass through while preventing larger molecules like plasma proteins and blood cells from entering the glomerular capsule. This process is driven by the net filtration pressure, which is the difference between glomerular blood hydrostatic pressure and the sum of capsular hydrostatic pressure and blood colloid osmotic pressure.
What is the glomerular filtration rate (GFR)?
The glomerular filtration rate (GFR) is the amount of filtrate formed by both kidneys per minute. It is a crucial measure of kidney function and overall health. In a healthy adult, the GFR is approximately 125 ml/minute, which amounts to an astounding 180 liters per day.
How is tubular reabsorption different from tubular secretion?
Tubular reabsorption involves the movement of substances from the filtrate back into the blood. This process ensures that essential nutrients, electrolytes, and water are retained in the body. In contrast, tubular secretion actively transports certain substances from the blood into the nephron to modify the composition of the filtrate. Tubular secretion is essential for maintaining ionic and acid-base balance in the body.
What are countercurrent mechanisms in the kidneys?
The kidneys employ countercurrent mechanisms, including countercurrent multiplication and countercurrent exchange, to create and maintain the osmotic gradient in the renal medulla. Countercurrent multiplication occurs in the long nephron loops of juxtamedullary nephrons and establishes the osmotic gradient. Countercurrent exchange occurs in the vasa recta, allowing for passive exchange of solutes and water between the blood and interstitial fluid in the medulla.
Why is urine formation important for the body?
Urine formation is vital for maintaining the body's internal environment and overall health. It helps eliminate waste products and excess substances from the body while retaining essential nutrients and maintaining the proper balance of ions and pH levels in the blood. Proper urine formation ensures the body's homeostasis and prevents the buildup of harmful substances in the bloodstream.