Table of Contents
Entamoeba histolytica has a global distribution, with a higher prevalence in tropical regions compared to other areas. It thrives in places where sanitation is inadequate. Entamoeba histolytica, a protozoan parasite, is the causal agent behind human amoebiasis. The trophozoites of E. histolytica inhabit the mucous and submucous layers of the large intestine in humans.
The systematic position of Entamoeba histolytica
- Phylum — Protozoa
- Sub phylum – Plasmodroma
- Class – Rhizopoda (Sarcodina)
- Order – Lobosa
- Sub-order – Nuda (Amoebina)
- Genus – Entamoeba
- Species — Histolytica
Mode of transmission
The infective stage of Entamoeba histolytica, characterised by a mature quadrinucleate cyst, is responsible for transmitting the parasite. The transmission of E. histolytica from one individual to another occurs through the ingestion of these cysts. The main sources of infection are faecal contamination of consumable items and drinking water. The most common mode of infection is faeco-oral route. The consumption of contaminated raw vegetables and fruits leads to amoebiasis. Insects such as flies, cockroaches, and rodents serve as carriers of the infective cysts, transferring them to food and beverages. Additionally, outbreaks can occur when the water supply becomes contaminated with cysts from infected fecal matter.
Morphology
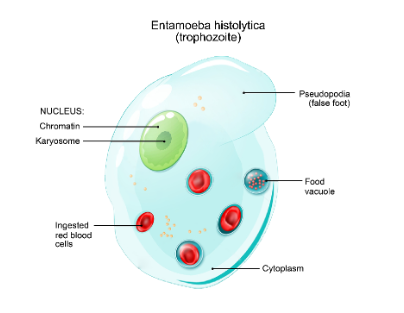
E. histolytica presents itself in three distinct forms: trophozoite, precyst, and cyst.
- Trophozoite
The trophozoite is the active feeding stage of the parasite. Found in the large intestine’s mucosa and sub-mucosa layers, these unicellular organisms measure 18 to 40 micrometers in diameter (average 20 to 30 um). They glide slowly with changing body shapes due to pseudopodia formation. The cytoplasm has clear ectoplasm and granular endoplasm housing a single nucleus, red blood cells, and debris. Trophozoites release a histolysin enzyme, causing tissue breakdown for absorption as food. Reproducing via binary fission, they multiply rapidly, relying on host tissues for growth.
- Pre cystic stage
The precystic stage serves as a transitional phase between the trophozoite and cystic stages within the parasite’s life cycle. In this phase, the parasite’s size diminishes (10-20 micrometers), its shape becomes more streamlined, and it develops a single blunt pseudopodium. Notably, the endoplasm no longer contains engulfed red blood cells (RBCs) or other cellular debris. This suggests a temporary cessation of feeding during this stage, while a solitary nucleus remains discernible.
- Cystic stage
Within the host’s intestinal lumen, the process of cyst formation takes place. The previously precystic parasite migrates into the gut lumen and undergoes a transformation into the cystic form, known as “encystation.” During encystation, the parasite adopts a rounded morphology and becomes enveloped by a distinctive double refractile wall referred to as the cyst wall.
Life cycle
- The life cycle of E. histolytica involves two distinct forms: the trophozoite, which is actively dividing, and the cyst, a dormant stage.
- Human infection typically initiates with the ingestion of cysts present in food or water contaminated with human faeces. Despite exposure to the stomach’s acidic environment, the cysts endure and advance to the intestine.
- Within the ileo-cecal region, the cysts undergo a process called excystment, yielding eight trophozoites from each cyst.
- These trophozoites migrate to the colon and proliferate. While often coexisting with the host as commensals within the intestine, trophozoites can alternatively launch attacks on and infiltrate the intestinal mucosa, potentially causing dysentery.
- Additionally, trophozoites can travel through the bloodstream to distant sites like the liver, brain, and lungs, inducing severe abscesses that endanger the host’s life.
- In the intestine, numerous trophozoites transform into cysts, generating quadrinucleated cysts.
- Both trophozoites and cysts exit the body via feces.
- While cysts can persist outside the host for extended periods, trophozoites have a limited survival span of a few hours. While trophozoites do not play a role in disease transmission, they are responsible for inflicting tissue damage.
- The primary reservoir for human infection is asymptomatic carriers who continuously shed cysts, inadvertently propagating the disease.
Pathology
The incubation period in humans, varying due to immune response, typically spans 4 to 5 days post-parasite infection. It gives rise to two distinct impacts:
- Intestinal or primary lesions, the initial infection predominantly affects the large intestine. Trophozoites, infiltrating the mucosa and submucosa, proliferate and erode intestinal tissues via the release of proteolytic enzymes. This results in multiple pathological conditions, including amoebic dysentery characterised by painful, frequent bowel movements accompanied by mucus and sporadic blood. Furthermore, amoebic ulcers emerge in the caecum, ascending colon, and rectum. In severe cases, intestinal wall perforation, gangrene, pericolic abscesses, and peritonitis can manifest.
- Metastatic or secondary lesions, chronic instances enable parasite entry into the bloodstream, propagating to various body parts and instigating extra-intestinal or metastatic lesions termed “tissue amoebiasis.” This encompasses hepatic amoebiasis marked by scattered tender liver abscesses, pulmonary amoebiasis involving single or multiple lung abscesses, cerebral amoebiasis with small abscesses in brain hemispheres, and rare splenic amoebiasis causing abscesses. Cutaneous lesions and urinogenital tract infections can also result.Amoebicidal drugs help in the treatment of amoebiasis.
Preventive measures
Personal Prophylaxis
- Avoiding raw fruits and vegetables.
- Consuming boiled drinking water.
- Safeguarding food and drinks from fly and cockroach contamination.
- Adhering to basic hygiene practices and maintaining personal cleanliness.
Community Prophylaxis
- Proper disposal of human excreta and practicing handwashing after defecation.
- Ensuring water supplies are protected from fecal contamination.
- Avoiding the use of fresh human feces as fertilizer.
- Educating the public about the parasite and its transmission methods.
Summary
Entamoeba histolytica, a protozoan parasite responsible for human amoebiasis, has a global distribution, prevalent in tropical regions with inadequate sanitation. Its life cycle involves three forms: trophozoite, precyst, and cyst. The transmission occurs through ingestion of mature quadrinucleate cysts, primarily via contaminated food, water, and fecal-oral route. Trophozoites inhabit the large intestine’s mucosa and sub-mucosa, causing disease through tissue destruction. The incubation period varies, leading to either primary lesions in the intestine like dysentery and ulcers or secondary lesions affecting distant organs. Treatment employs amoebicidal drugs. Preventive measures include personal hygiene and sanitation practices along with public awareness about the parasite and its transmission.
FAQs on Amoebiasis
What is Entamoeba histolytica?
Entamoeba histolytica is a protozoan parasite responsible for causing human amoebiasis, a disease prevalent in tropical regions with poor sanitation.
How does Entamoeba histolytica spread?
The parasite spreads through the ingestion of mature quadrinucleate cysts found in contaminated food, water, and through the fecal-oral route.
What are the different forms of Entamoeba histolytica?
Entamoeba histolytica exists in three forms: trophozoite, precyst, and cyst. Trophozoites actively feed in the large intestine's mucous and submucous layers, while precyst and cyst stages play roles in the parasite's life cycle.
What are the symptoms and impacts of Entamoeba histolytica infection?
The infection's impact can be categorized into primary (intestinal) and secondary (metastatic) lesions. Primary lesions involve conditions like dysentery and ulcers, causing pain and discomfort in the large intestine. Secondary lesions affect organs such as the liver, lungs, brain, and spleen, potentially leading to abscesses.
How is Entamoeba histolytica infection treated?
Treatment involves the use of amoebicidal drugs to eliminate the parasite from the body.
How can Entamoeba histolytica infection be prevented?
Preventive measures include personal hygiene practices like avoiding raw fruits and vegetables, consuming boiled drinking water, and protecting food from contamination. Proper disposal of human waste, clean water supplies, and public education about transmission are crucial for community prevention.
What is the incubation period for Entamoeba histolytica infection?
he incubation period varies, typically lasting 4 to 5 days post-infection, before symptoms appear.
Can Entamoeba histolytica infections be fatal?
Yes, in severe cases, the infection can lead to life-threatening complications, especially when it spreads to other organs.
Who is most at risk for Entamoeba histolytica infection?
Individuals in areas with poor sanitation, particularly in tropical regions, are at higher risk due to increased exposure to contaminated food, water, and inadequate hygiene practices.